Medicine
From Wikipedia, the free encyclopedia

Medicine is the art and science of healing. It encompasses a range of health care practices evolved to maintain and restore health by the prevention and treatment of illness.
Contemporary medicine applies health science, biomedical research, and medical technology to diagnose and treat injury and disease, typically through medication, surgery, or some other form of therapy. The word medicine is derived from the Latin ars medicina, meaning the art of healing.[1][2]
Though medical technology and clinical expertise are pivotal to contemporary medicine, successful face-to-face relief of actual suffering continues to require the application of ordinary human feeling and compassion, known in English as bedside manner.[3]
Contents[hide]
|
[edit] History

Prehistoric medicine incorporated plants (herbalism), animal parts and minerals. In many cases these materials were used ritually as magical substances by priests, shamans, or medicine men. Well-known spiritual systems include animism (the notion of inanimate objects having spirits), spiritualism (an appeal to gods or communion with ancestor spirits); shamanism (the vesting of an individual with mystic powers); and divination (magically obtaining the truth). The field of medical anthropology examines the ways in which culture and society are organized around or impacted by issues of health, health care and related issues.
Early records on medicine have been discovered from early Ayurvedic medicine in the Indian subcontinent, ancient Egyptian medicine, traditional Chinese medicine and ancient Greek medicine. Earliest records of dedicated hospitals come from Mihintale in Sri Lanka where evidence of dedicated medicinal treatment facilities for patients are found.[4][5] Early Greek doctor Hippocrates, who is called the Father of Medicine,[6][7] and Galen laid a foundation for later developments in a rational approach to medicine. After the fall of the Western Roman Empire and the onset of the Dark Ages, the Greek tradition of medicine went into decline in Western Europe, although it continued uninterrupted in the Easern Roman Empire (Byzantium). After 750, the Muslim Arab world had Hippocrates' and Galen's works translated into Arabic, and Islamic physicians engaged in some significant medical research. Notable Islamic medical pioneers include polymath Avicenna, who, along with Hippocrates, has also been called the Father of Medicine,[8][9] Abulcasis, the father of surgery, Avenzoar, the father of experimental surgery, Ibn al-Nafis, the father of circulatory physiology, and Averroes.[10] Rhazes, who is called the father of pediatrics, was one of first to question the Greek theory of humorism, which nevertheless remained influential in both medieval Western and medieval Islamic medicine [11] During the Crusades, one Muslim observer famously expressed a dim view of contemporary Western medicine.[12] However, overall mortality and mordibity levels in the medieval Middle East and medieval Europe did not significantly differ one from the other, which indicates that there was no major medical "breakthrough" to modern medicine in either region in this period. The fourteenth and fifteenth century Black Death was just as devastating to the Middle East as to Europe, and it has even been argued that Western Europe was generally more effective in recovering from the pandemic than the Middle East.[13] In the early modern period, important early figures in medicine and anatomy emerged in Europe, including Gabriele Falloppio and William Harvey.

The major shift in medical thinking was the gradual rejection, especially during the Black Death in the 14th and 15th centuries, of what may be called the 'traditional authority' approach to science and medicine. This was the notion that because some prominent person in the past said something must be so, then that was the way it was, and anything one observed to the contrary was an anomaly (which was paralleled by a similar shift in European society in general - see Copernicus's rejection of Ptolemy's theories on astronomy). Physicians like Ibn al-Nafis and Vesalius improved upon or indeed rejected the theories of great authorities from the past (such as Hippocrates, and Galen), many of whose theories were in time discredited.
Modern scientific biomedical research (where results are testable and reproducible) began to replace early Western traditions based on herbalism, the Greek "four humours" and other such pre-modern notions. The modern era really began with Robert Koch's discoveries around 1880 of the transmission of disease by bacteria, and then the discovery of antibiotics around 1900. The post-18th century modernity period brought more groundbreaking researchers from Europe. From Germany and Austrian doctors such as Rudolf Virchow, Wilhelm Conrad Röntgen, Karl Landsteiner, and Otto Loewi) made contributions. In the United Kingdom Alexander Fleming, Joseph Lister, Francis Crick, and Florence Nightingale are considered important. From New Zealand and Australia came Maurice Wilkins, Howard Florey, and Frank Macfarlane Burnet). In the United States William Williams Keen, Harvey Cushing, William Coley, James D. Watson, Italy (Salvador Luria), Switzerland (Alexandre Yersin), Japan (Kitasato Shibasaburo), and France (Jean-Martin Charcot, Claude Bernard, Paul Broca and others did significant work. Russian (Nikolai Korotkov also did significant work, as did Sir William Osler and Harvey Cushing.
As science and technology developed, medicine became more reliant upon medications. Throughout history and in Europe right until the late 18th century not only animal and plant products were used as medicine, but also human body parts and fluids.[14] Pharmacology developed from herbalism and many drugs are still derived from plants (atropine, ephedrine, warfarin, aspirin, digoxin, vinca alkaloids, taxol, hyoscine, etc). The first of these was arsphenamine / Salvarsan discovered by Paul Ehrlich in 1908 after he observed that bacteria took up toxic dyes that human cells did not. Vaccines were discovered by Edward Jenner and Louis Pasteur. The first major class of antibiotics was the sulfa drugs, derived by French chemists originally from azo dyes. This has become increasingly sophisticated; modern biotechnology allows drugs targeted towards specific physiological processes to be developed, sometimes designed for compatibility with the body to reduce side-effects. Genomics and knowledge of human genetics is having some influence on medicine, as the causative genes of most monogenic genetic disorders have now been identified, and the development of techniques in molecular biology and genetics are influencing medical technology, practice and decision-making.
Evidence-based medicine is a contemporary movement to establish the most effective algorithms of practice (ways of doing things) through the use of systematic reviews and meta-analysis. The movement is facilitated by the modern global information science, which allows all evidence to be collected and analyzed according to standard protocols which are then disseminated to healthcare providers. One problem with this 'best practice' approach is that it could be seen to stifle novel approaches to treatment. The Cochrane Collaboration leads this movement. A 2001 review of 160 Cochrane systematic reviews revealed that, according to two readers, 21.3% of the reviews concluded insufficient evidence, 20% concluded evidence of no effect, and 22.5% concluded positive effect.[15]
[edit] Clinical practice

In clinical practice doctors personally assess patients in order to diagnose, treat, and prevent disease using clinical judgment. The doctor-patient relationship typically begins an interaction with an examination of the patient's medical history and medical record, followed a medical interview[16] and a physical examination. Basic diagnostic medical devices (e.g. stethoscope, tongue depressor) are typically used. After examination for signs and interviewing for symptoms, the doctor may order medical tests (e.g. blood tests), take a biopsy, or prescribe pharmaceutical drugs or other therapies. Differential diagnosis methods help to rule out conditions based on the information provided. During the encounter, properly informing the patient of all relevant facts is an important part of the relationship and the development of trust. The medical encounter is then documented in the medical record, which is a legal document in many jurisdictions.[17] Followups may be shorter but follow the same general procedure.
The components of the medical interview[16] and encounter are:
- Chief complaint (cc): the reason for the current medical visit. These are the 'symptoms.' They are in the patient's own words and are recorded along with the duration of each one. Also called 'presenting complaint.'
- History of present illness / complaint (HPI): the chronological order of events of symptoms and further clarification of each symptom.
- Current activity: occupation, hobbies, what the patient actually does.
- Medications (Rx): what drugs the patient takes including prescribed, over-the-counter, and home remedies, as well as alternative and herbal medicines/herbal remedies. Allergies are also recorded.
- Past medical history (PMH/PMHx): concurrent medical problems, past hospitalizations and operations, injuries, past infectious diseases and/or vaccinations, history of known allergies.
- Social history (SH): birthplace, residences, marital history, social and economic status, habits (including diet, medications, tobacco, alcohol).
- Family history (FH): listing of diseases in the family that may impact the patient. A family tree is sometimes used.
- Review of systems (ROS) or systems inquiry: a set of additional questions to ask which may be missed on HPI: a general enquiry (have you noticed any weight loss, change in sleep quality, fevers, lumps and bumps? etc), followed by questions on the body's main organ systems (heart, lungs, digestive tract, urinary tract, etc).
The physical examination is the examination of the patient looking for signs of disease ('Symptoms' are what the patient volunteers, 'Signs' are what the healthcare provider detects by examination). The healthcare provider uses the senses of sight, hearing, touch, and sometimes smell (taste has been made redundant by the availability of modern lab tests). Four chief methods are used: inspection, palpation (feel), percussion (tap to determine resonance characteristics), and auscultation (listen); smelling may be useful (e.g. infection, uremia, diabetic ketoacidosis). The clinical examination involves study of:
- Vital signs including height, weight, body temperature, blood pressure, pulse, respiration rate, hemoglobin oxygen saturation
- General appearance of the patient and specific indicators of disease (nutritional status, presence of jaundice, pallor or clubbing)
- Skin
- Head, eye, ear, nose, and throat (HEENT)
- Cardiovascular (heart and blood vessels)
- Respiratory (large airways and lungs)
- Abdomen and rectum
- Genitalia (and pregnancy if the patient is or could be pregnant)
- Musculoskeletal (including spine and extremities)
- Neurological (consciousness, awareness, brain, vision, cranial nerves, spinal cord and peripheral nerves)
- Psychiatric (orientation, mental state, evidence of abnormal perception or thought)
Laboratory and imaging studies results may be obtained, if necessary.
The medical decision-making (MDM) process involves analysis and synthesis of all the above data to come up with a list of possible diagnoses (the differential diagnoses), along with an idea of what needs to be done to obtain a definitive diagnosis that would explain the patient's problem.
The treatment plan may include ordering additional laboratory tests and studies, starting therapy, referral to a specialist, or watchful observation. Follow-up may be advised.
This process is used by primary care providers as well as specialists. It may take only a few minutes if the problem is simple and straightforward. On the other hand, it may take weeks in a patient who has been hospitalized with bizarre symptoms or multi-system problems, with involvement by several specialists.
On subsequent visits, the process may be repeated in an abbreviated manner to obtain any new history, symptoms, physical findings, and lab or imaging results or specialist consultations.
[edit] Institutions
Contemporary medicine is in general conducted within health care systems. Legal, credentialing and financing frameworks are established by individual governments, augmented on occasion by international organizations. The characteristics of any given health care system have significant impact on the way medical care is provided.
Advanced industrial countries (with the exception of the United States) [18][19] and many developing countries provide medical services though a system of universal health care which aims to guarantee care for all through a single-payer health care system, or compulsory private or co-operative health insurance. This is intended to ensure that the entire population has access to medical care on the basis of need rather than ability to pay. Delivery may be via private medical practices or by state-owned hospitals and clinics, or by charities; most commonly by a combination of all three.
Most tribal societies, but also some communist countries (e.g. China) and the United States,[18][19] provide no guarantee of health care for the population as a whole. In such societies, health care is available to those that can afford to pay for it or have self insured it (either directly or as part of an employment contract) or who may be covered by care financed by the government or tribe directly.

Transparency of information is another factor defining a delivery system. Access to information on conditions, treatments, quality and pricing greatly affects the choice by patients / consumers and therefore the incentives of medical professionals. While the US health care system has come under fire for lack of openness,[20] new legislation may encourage greater openness. There is a perceived tension between the need for transparency on the one hand and such issues as patient confidentiality and the possible exploitation of information for commercial gain on the other.
[edit] Delivery
Provision of medical care is classified into primary, secondary and tertiary care categories.
Primary care medical services are provided by physicians, physician assistants,Nurse Practitioners, or other health professionals who have first contact with a patient seeking medical treatment or care. These occur in physician offices, clinics, nursing homes, schools, home visits and other places close to patients. About 90% of medical visits can be treated by the primary care provider. These include treatment of acute and chronic illnesses, preventive care and health education for all ages and both sexes.
Secondary care medical services are provided by medical specialists in their offices or clinics or at local community hospitals for a patient referred by a primary care provider who first diagnosed or treated the patient. Referrals are made for those patients who required the expertise or procedures performed by specialists. These include both ambulatory care and inpatient services, emergency rooms, intensive care medicine, surgery services, physical therapy, labor and delivery, endoscopy units, diagnostic laboratory and medical imaging services, hospice centers, etc. Some primary care providers may also take care of hospitalized patients and deliver babies in a secondary care setting.
Tertiary care medical services are provided by specialist hospitals or regional centers equipped with diagnostic and treatment facilities not generally available at local hospitals. These include trauma centers, burn treatment centers, advanced neonatology unit services, organ transplants, high-risk pregnancy, radiation oncology, etc.
Modern medical care also depends on information - still delivered in many health care settings on paper records, but increasingly nowadays by electronic means.
[edit] Branches
Working together as an interdisciplinary team, many highly-trained health professionals besides medical practitioners are involved in the delivery of modern health care. Examples include: nurses, emergency medical technicians and paramedics, laboratory scientists, (pharmacy, pharmacists), (physiotherapy,physiotherapists), respiratory therapists, speech therapists, occupational therapists, radiographers, dietitians and bioengineers.
The scope and sciences underpinning human medicine overlap many other fields. Dentistry, while a separate discipline from medicine, is considered a medical field.
A patient admitted to hospital is usually under the care of a specific team based on their main presenting problem, e.g. the Cardiology team, who then may interact with other specialties, e.g. surgical, radiology, to help diagnose or treat the main problem or any subsequent complications / developments.
Physicians have many specializations and subspecializations into certain branches of medicine, which are listed below. There are variations from country to country regarding which specialties certain subspecialties are in.
The main branches of medicine used in Wikipedia are:
- Basic sciences of medicine; this is what every physician is educated in, and some return to in biomedical research.
- Medical specialties
- interdisciplinary fields, where different medical specialties are mixed to function in certain occasions.
[edit] Basic sciences
- Anatomy is the study of the physical structure of organisms. In contrast to macroscopic or gross anatomy, cytology and histology are concerned with microscopic structures.
- Biochemistry is the study of the chemistry taking place in living organisms, especially the structure and function of their chemical components.
- Biostatistics is the application of statistics to biological fields in the broadest sense. A knowledge of biostatistics is essential in the planning, evaluation, and interpretation of medical research. It is also fundamental to epidemiology and evidence-based medicine.
- Cytology is the microscopic study of individual cells.
- Embryology is the study of the early development of organisms.
- Epidemiology is the study of the demographics of disease processes, and includes, but is not limited to, the study of epidemics.
- Genetics is the study of genes, and their role in biological inheritance.
- Histology is the study of the structures of biological tissues by light microscopy, electron microscopy and immunohistochemistry.
- Immunology is the study of the immune system, which includes the innate and adaptive immune system in humans, for example.
- Medical physics is the study of the applications of physics principles in medicine.
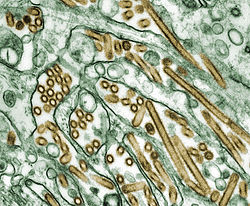
- Microbiology is the study of microorganisms, including protozoa, bacteria, fungi, and viruses.
- Neuroscience includes those disciplines of science that are related to the study of the nervous system. A main focus of neuroscience is the biology and physiology of the human brain and spinal cord.
- Nutrition science (theoretical focus) and dietetics (practical focus) is the study of the relationship of food and drink to health and disease, especially in determining an optimal diet. Medical nutrition therapy is done by dietitians and is prescribed for diabetes, cardiovascular diseases, weight and eating disorders, allergies, malnutrition, and neoplastic diseases.
- Pathology as a science is the study of disease—the causes, course, progression and resolution thereof.
- Pharmacology is the study of drugs and their actions.
- Physiology is the study of the normal functioning of the body and the underlying regulatory mechanisms.
- Toxicology is the study of hazardous effects of drugs and poisons.
[edit] Specialties
In the broadest meaning of "medicine", there are many different specialties. However, within medical circles, there are two broad categories: "Medicine" and "Surgery." "Medicine" refers to the practice of non-operative medicine, and most subspecialties in this area require preliminary training in "Internal Medicine". "Surgery" refers to the practice of operative medicine, and most subspecialties in this area require preliminary training in "General Surgery." There are some specialties of medicine that do not fit into either of these categories, such as radiology, pathology, or anesthesia, and those are also discussed further below.
[edit] Surgery
Surgical specialties employ operative treatment. In addition, surgeons must decide when an operation is necessary, and also treat many non-surgical issues, particularly in the surgical intensive care unit (SICU), where a variety of critical issues arise. Surgery has many subspecialties, e.g. general surgery, transplant surgery, trauma surgery, cardiovascular surgery, neurosurgery, maxillofacial surgery, orthopedic surgery, otolaryngology, plastic surgery, oncologic surgery, vascular surgery, and pediatric surgery. In some centers, anesthesiology is part of the division of surgery (for logistical and planning purposes), although it is not a surgical discipline.
Surgical training in the U.S. requires a minimum of five years of residency after medical school. Sub-specialties of surgery often require seven or more years. In addition, fellowships can last an additional one to three years. Because post-residency fellowships can be competitive, many trainees devote two additional years to research. Thus in some cases surgical training will not finish until more than a decade after medical school. Furthermore, surgical training can be very difficult and time consuming.
[edit] 'Medicine' as a specialty
Internal medicine is the medical specialty concerned with the diagnosis, management and nonsurgical treatment of unusual or serious diseases, either of one particular organ system or of the body as a whole. According to some sources, an emphasis on internal structures is implied.[21] In North America, specialists in internal medicine are commonly called "internists". Elsewhere, especially in Commonwealth nations, such specialists are often called physicians.[22] These terms, internist or physician (in the narrow sense, common outside North America), generally exclude practitioners of gynecology and obstetrics, pathology, psychiatry, and especially surgery and its subspecialities.
Because their patients are often seriously ill or require complex investigations, internists do much of their work in hospitals. Formerly, many internists were not subspecialized; such general physicians would see any complex nonsurgical problem; this style of practice has become much less common. In modern urban practice, most internists are subspecialists: that is, they generally limit their medical practice to problems of one organ system or to one particular area of medical knowledge. For example, gastroenterologists and nephrologists specialize respectively in diseases of the gut and the kidneys.[23]
In Commonwealth and some other countries, specialist pediatricians and geriatricians are also described as specialist physicians (or internists) who have subspecialized by age of patient rather than by organ system. Elsewhere, especially in North America, general pediatrics is often a form of Primary care.
There are many subspecialities (or subdisciplines) of internal medicine:
-
- Cardiology
- Critical care medicine
- Dermatology
- Emergency medicine
- Endocrinology
- Gastroenterology
- Geriatrics
- Haematology
- Hepatology
- Infectious diseases
- Nephrology
- Neurology
- Oncology
- Pediatrics
- Pulmonology
- Rheumatology
- Sleep medicine
Training in internal medicine (as opposed to surgical training), varies considerably across the world: see the articles on Medical education and Physician for more details. In North America, it requires at least three years of residency training after medical school, which can then be followed by a one to three year fellowship in the subspecialties listed above. In general, resident work hours in medicine are less than those in surgery, averaging about 60 hours per week in the USA.